Finding the Right MCAS Specialist: A Guide to the Best MCAS Doctors and Treatment Options
Mast Cell Activation Syndrome (MCAS) is a complex, often misunderstood condition that can cause a wide range of symptoms and severely affect quality of life. With MCAS becoming more recognized in the medical community, patients are increasingly seeking knowledgeable, specialized care. If you’re searching for a MCAS specialist, wondering who the best MCAS doctors are, or exploring MCAS treatment options, this comprehensive guide will answer your questions and help you take the next step toward effective management.
What is Mast Cell Activation Syndrome (MCAS)?
MCAS is a chronic condition where mast cells inappropriately and excessively release chemical mediators, leading to symptoms affecting multiple organ systems. Unlike mastocytosis, which involves an abnormal increase in the number of mast cells, MCAS is about dysfunctional mast cell activation.
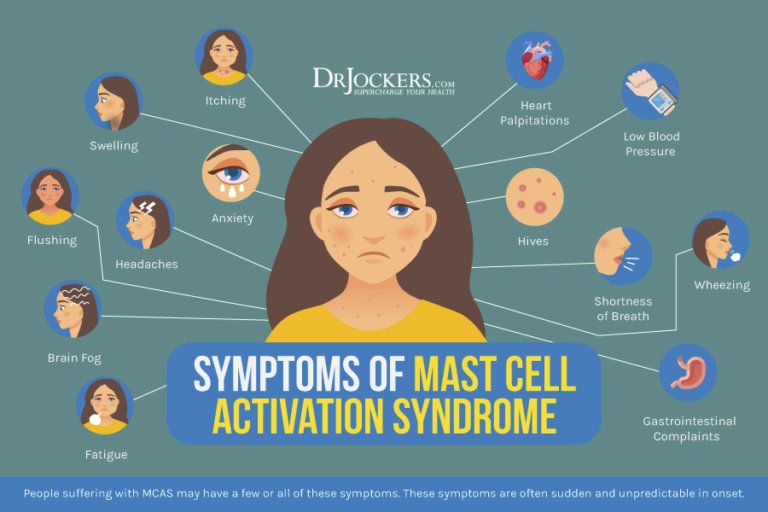
Common Symptoms of MCAS
- Chronic fatigue
- Abdominal pain, bloating, or diarrhea
- Skin rashes or flushing
- Headaches or migraines
- Brain fog
- Rapid heart rate or low blood pressure
- Wheezing or shortness of breath
- Anaphylaxis or allergic-like reactions
Because symptoms mimic those of other conditions, patients are often misdiagnosed or go undiagnosed for years. That’s why seeking an experienced MCAS specialist is essential.
Why You Need a Specialist for MCAS
General practitioners or even some allergists may not be equipped to recognize or treat MCAS. A MCAS specialist has specific training and experience in mast cell disorders, which allows for more accurate diagnosis and personalized treatment strategies.
The Role of an MCAS Specialist
- Ordering and interpreting specialized lab tests (e.g., serum tryptase, 24-hour urinary histamine)
- Differentiating MCAS from other similar conditions
- Creating individualized treatment plans based on symptom patterns and test results
- Monitoring responses to treatment and adjusting medications as needed
- Educating patients on lifestyle modifications and trigger avoidance
What to Look for in the Best MCAS Doctors
Finding the best MCAS doctors involves more than just credentials. Consider the following when evaluating a potential provider:
1. Experience with Mast Cell Disorders
Look for doctors who have diagnosed and treated multiple MCAS cases and are familiar with up-to-date clinical research.
2. Multidisciplinary Approach
MCAS affects various body systems, so the best doctors often collaborate with immunologists, gastroenterologists, dermatologists, and neurologists.
3. Personalized Care
Every patient presents differently. The top MCAS doctors tailor treatment plans based on individual needs rather than using a one-size-fits-all approach.
4. Patient Education
Trustworthy specialists take time to educate patients about their condition, helping them understand triggers, medications, and long-term management.
Diagnosing MCAS: The First Step Toward Healing
The diagnostic process for MCAS can be tricky. There’s no single test to confirm it. Instead, diagnosis is usually based on three criteria:
- Clinical symptoms consistent with mast cell activation.
- Laboratory evidence of increased mast cell mediators.
- Improvement of symptoms with medications that block or reduce mast cell activation.
Some of the key tests may include:
- Plasma histamine levels
- Serum tryptase
- 24-hour urine tests for prostaglandin D2 and N-methylhistamine
- Chromogranin A levels
An experienced MCAS specialist will know how to order and interpret these tests properly, even when results are borderline or inconsistent.
MCAS Treatment Options: A Multifaceted Approach
Effective MCAS treatment isn’t about curing the condition—it’s about managing symptoms, reducing flares, and improving quality of life. Treatment typically includes a combination of medications, lifestyle changes, and trigger avoidance.
Medications for MCAS
- Antihistamines (H1 and H2 blockers): Loratadine, cetirizine, famotidine
- Mast cell stabilizers: Cromolyn sodium, ketotifen
- Leukotriene inhibitors: Montelukast
- Aspirin (low dose): Helps reduce prostaglandin levels in some patients
- Steroids: Short-term use in severe cases
- Epinephrine auto-injectors: For patients at risk of anaphylaxis
Each patient may respond differently to medications, so treatment must be fine-tuned over time.
Dietary Adjustments
Some foods can trigger mast cell degranulation. A low-histamine diet is often recommended, focusing on:
- Fresh-cooked meats
- Non-citrus fruits
- Gluten-free grains
- Avoiding leftovers, aged cheeses, alcohol, fermented foods, and canned items
Working with a nutritionist familiar with MCAS can make dietary transitions smoother and more effective.
Environmental and Lifestyle Modifications
- Avoid strong scents, cigarette smoke, and chemical cleaners
- Manage stress through meditation, yoga, or therapy
- Use air purifiers to reduce allergens
- Keep temperature and humidity stable
How to Find the Best MCAS Specialists Near You
Because MCAS is still an emerging field, specialists are often located at academic medical centers or in integrative practices. Here are some strategies for finding top providers:
- Search patient forums and support groups – Communities like MastAttack, The Mast Cell Disease Society, and Inspire MCAS groups often share experiences and recommendations.
- Check academic hospital directories – Leading centers in immunology or allergy research may list mast cell specialists.
- Ask your primary doctor for a referral – A knowledgeable physician might help you connect with a reputable specialist.
- Use telemedicine options – Some of the best MCAS doctors now offer virtual consultations, expanding access regardless of location.
Living with MCAS: Building a Supportive Environment
One of the hardest parts of living with MCAS is the unpredictability. Flares can come without warning, and triggers may be hard to identify. Emotional support, awareness, and advocacy play a big role in long-term wellbeing.
Tips for Daily Life with MCAS
- Keep a symptom and food diary to track flares
- Educate family and friends about the condition so they can be supportive
- Prepare an emergency kit with meds and epinephrine if needed
- Advocate for accommodations at work or school when necessary
- Join support groups to connect with others facing similar challenges
MCAS doesn’t have to define your life. With the right treatment and support, it is possible to live well.