Automating Denial Management: A Game Changer for Healthcare Providers
It is a known fact that healthcare providers struggle with managing claims and denials due to the scale and complexity of the processes involved. Hence, it is essential to streamline the claim denials process of the revenue cycle for better operational efficiency. Traditionally, it is a long way toward simplifying the denial management process. However, denial management automation can offer more efficient strategies.
The denial management process can range from identifying and addressing claim denials to preventing the same case from happening in the future. Manually doing these tasks has been time-consuming and labor-intensive. Automating this process can avoid human errors and reduce the long hours that healthcare spends on administrative legwork rather than concentrating on the patient’s welfare.
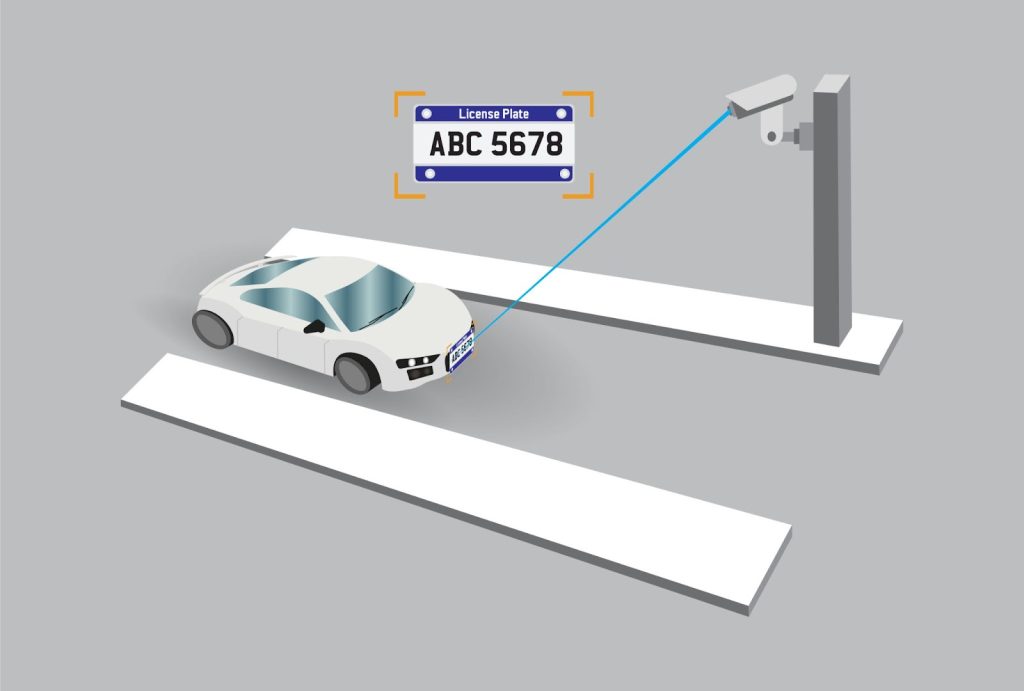
Healthcare processes can be complex, and navigating through such systems requires well-designed automation strategies to achieve the best results. Integrating artificial intelligence and machine learning can help create advanced solutions for unique cases based on the everyday occurrences at your practice.
Claim Denials and The Challenges Faced Today
The number of claim denials has risen, and the trend only worsens. What is causing this surge? Here are some facts about the global rise in denial rates over the past year.
There is a 23% increase in claim denials. However, the good news is that 90% of them are preventable.
Denial Management Automation
While many healthcare organizations still depend on staff to do their daily administrative tasks, automation can significantly transform the denial management process more efficiently.
- Automating low-impact, high-volume denials can unlock the potential of the staff, allowing them to utilize their time for patient care.
- Automatically eliminating duplicate denials when the existing denial is paid for.
- Preventing denials caused due to non-coverage by prior identification.
- Automating account transactions and transfers.
Best Practices in Denial Management Framework
A well-designed denial management automation system will have a defined workflow by integrating analytics into doable solutions to prevent future denials.
Here are some best practices:
- Understanding and identifying the denial patterns: It is essential to analyze and identify the root cause for claim denials by learning more about the matched claim and remit schemes. This is to determine the common reasons for denials and avoid them in the future.
- Gathering denial appeals data: Traditionally, a staff team gathered patient data on denial appeals and analyzed the core nuances. Denial management system can generate predictive reports based on the outcome of the denial appeals process.
- Real–time reporting: Leveraging AI and ML to produce accurate reports based on real-time analytics helps derive actionable insights for the denial management process. These reports help healthcare practitioners to take proactive measures to prevent and manage claim denials efficiently.
- Categorize the denials: To predict denials and avoid them from happening in the future, it is essential to understand the root cause. Denials in medical billing can occur due to various reasons. Integrating automation in denial management can help organize and prioritize claims based on the propensity of payment.
- Streamlining Workflows: Denial Management Automation can categorize the denials based on specific physicians, payers, CPT codes, and various other factors based on the practice’s requirements. Once identified, these patterns can be instrumental in designing strategies to improve and address any future concerns.
Wrapping Up
As the future of healthcare becomes more digital, denial management automation plays a vital role in enhancing the revenue cycle. Leveraging advanced technology such as AI, ML, and predictive analytics will educate these systems to reduce claims denials before they occur and improve the overall operational and financial efficiency of healthcare organizations.
Expect to see even more advanced strategies in denial management automation with the integration of revenue cycle management solutions, resulting in end-to-end automation. These adaptations will capacitate healthcare providers to indulge in patient care and welfare while allowing automated systems to take care of their legwork.
At Droidal, we are adopting advanced technologies to offer solutions for greater efficiency, accuracy, and financial stability, tailored specifically for your organization. As the healthcare industry continues to transform every day, our experts can help you embrace automation and take denial management to the next level. Connect with us today for a demo.
Also Read:
How to Submit an App on Google Play: A Simple Guide for Beginners










Post Comment